MAINE, USA — The coronavirus pandemic is not just a physical health crisis – it’s also a mental health crisis for people around the world. For some, like those struggling with substance abuse and recovery, the social isolation of the past few months has been tough to manage.
According to a recent study by drugabuse.com, 47 percent of Mainers are worried that the economic stress brought on by COVID-19 could result in more drug and alcohol use in their communities. This survey of 3,000 Americans also indicates that one in four Americans have noticed their neighbors drinking more alcohol since the beginning of lock-down. That’s why there are a number of initiatives happening around the state to aid in the prevention and treatment of addiction.
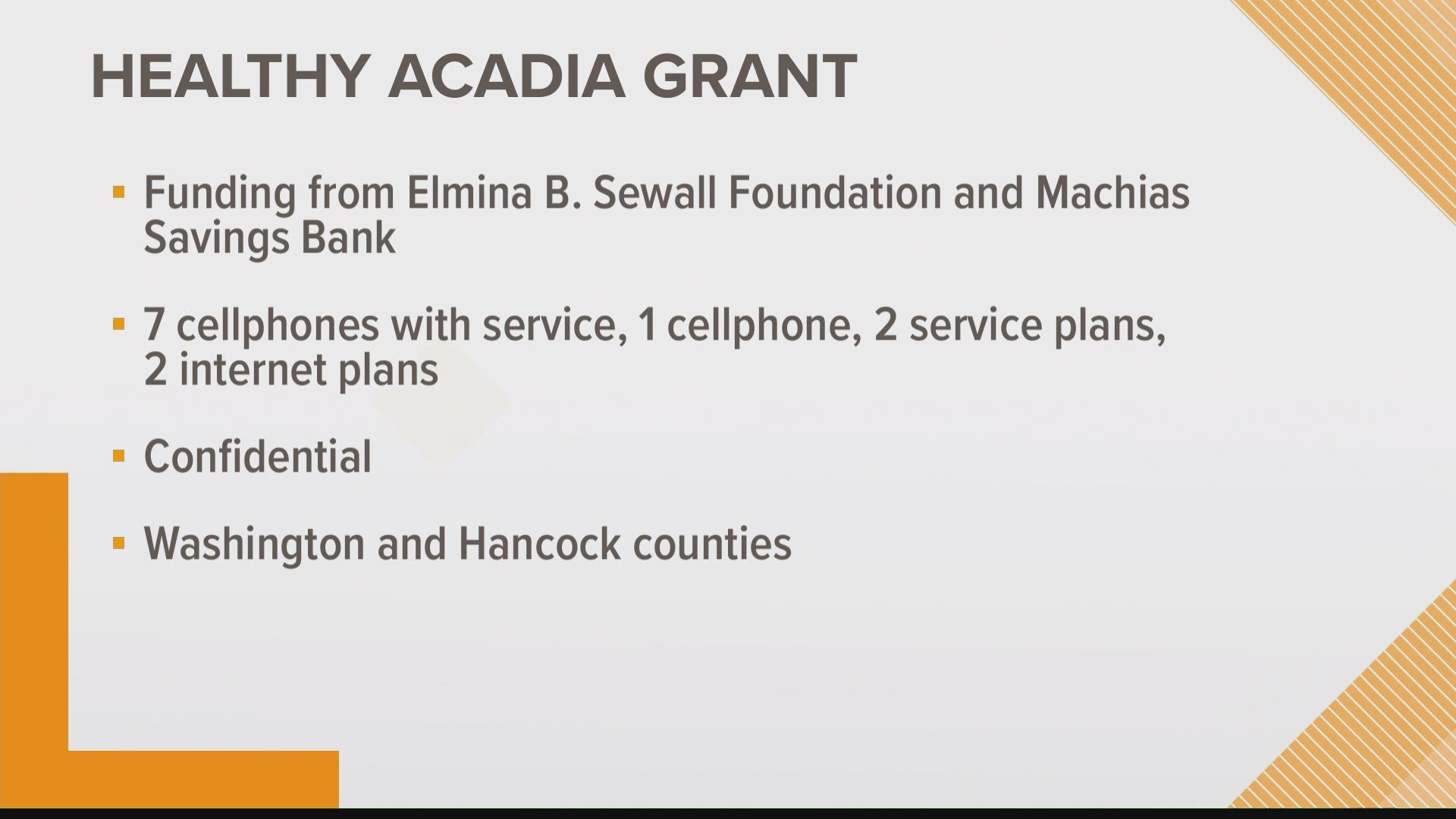
At the end of July, Healthy Acadia received funding from the Elmina B. Sewall Foundation and Machias Savings Bank to buy cellphones, service plans, and internet for people in recovery struggling with connectivity. Beth Alteri, a recovery volunteer coordinator for Healthy Acadia, says basically all services for people in recovery went remote when COVID-19 concerns crept into the state – and not everyone has access to a reliable phone, phone service, or internet to reach remote options.
Alteri says Healthy Acadia has ordered cellphones through U.S. Cellular, actually finding someone in recovery at the company, who was excited to help them with the project. As of August 25, Healthy Acadia had gifted seven cellphones with service, one cellphone without service, two service plans, and two internet packages. What individuals receive depends on their need, since each application is considered on an individual basis.
“That accountability is key. That support is key,” Alteri said about the importance of support networks when in recovery. “Being able to be connected to people in the recovery community is key for success, and when you lose that, we have to come up with creative ways to make sure that people who are in recovery are supported and not just feeling like they’re alone.”
Anyone in Hancock and Washington counties can apply, and Alteri says the program is completely confidential.
Another slightly different initiative with similar goals is happening in Dexter at Hometown Health Center. The clinic applied and was approved for a grant via UCLA and Dartmouth College to take part in a program that uses telehealth with patients struggling with opioid addiction. Through online health care provider Bright Heart Health, patients are able to reach medication-assisted treatment, counseling, and group visits – all with 24/7 access.
Funding for the project comes from the National Institute of Drug Abuse and is $125,000 for the first year to help HHC staff members attend meetings, go to conferences, market, and create reports. The study will last five years, and patients who take part will be compensated with about $255 for nine surveys total.
The program is entirely confidential. Patients can connect to the telehealth product on their own devices or in the Dexter office on an iPad, if they don’t have resources to connect elsewhere. HHC staff members say opioid addiction is a big problem in Maine, with about two people dying of an overdose every day. In their rural community, they say patients sometimes have to wait months to get into programs – and travel can be an issue, too.
“They are limited with transportation. They are even limited sometimes with cellphones because they have them sometimes, and then when they can’t pay for it, they don’t have that connection,” Mary Fitzgerald, a patient specialist at HHC, explained to NEWS CENTER Maine. “To rely on family members or friends – that makes it very difficult, too.”
“Traditionally in our medical facilities, you know, it’s very restrictive of the hours you get – but by having the telehealth, that patient, if they’re having a crisis, if they just need somebody to talk to, they can get access immediately,” HHC CEO Robin Winslow also noted.
This study is designed to determine whether adding telehealth programs to rural areas makes sense, based on how successful patients are. It went live July 6, and only two people are taking part at this point. HHC says they hope to have 40 participants in six months’ time.
To learn more, call HHC at 1-866-364-1366.